Our guest today is Rachael Rose, speech-language pathologist and owner of Creative Speech Therapy in Manhattan. We discuss the identification and treatment of tethered oral tissues (TOTs) in infants, more commonly known as tongue ties and lip ties, and their impact on feeding, speech, and overall development. Rachael explains the importance of early detection and intervention to prevent long-term issues, the importance of trusting parental intuition, the need for a supportive team approach, and the challenges parents face in getting proper diagnosis and treatment.
Resources:
Creative Speech Therapy - Rachael Rose
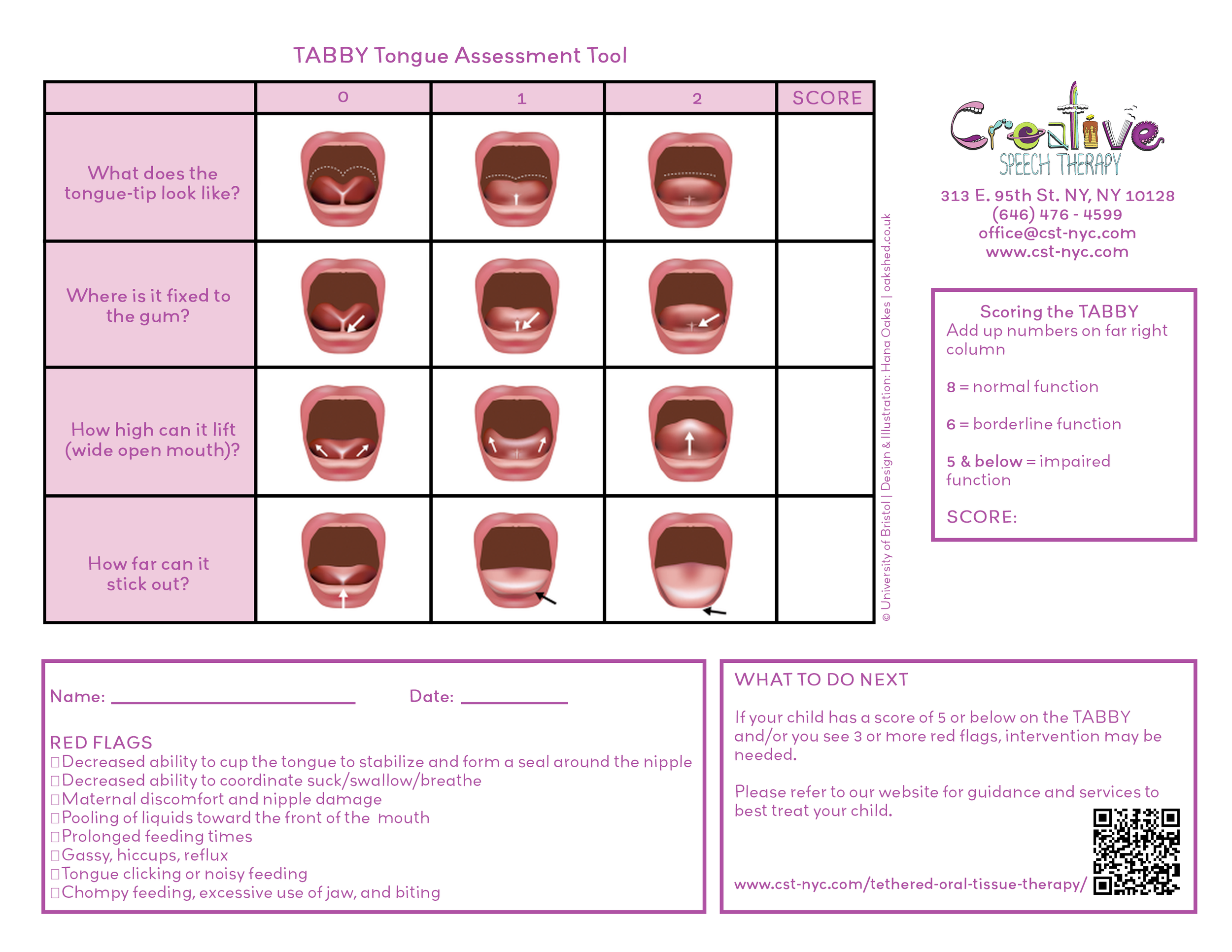
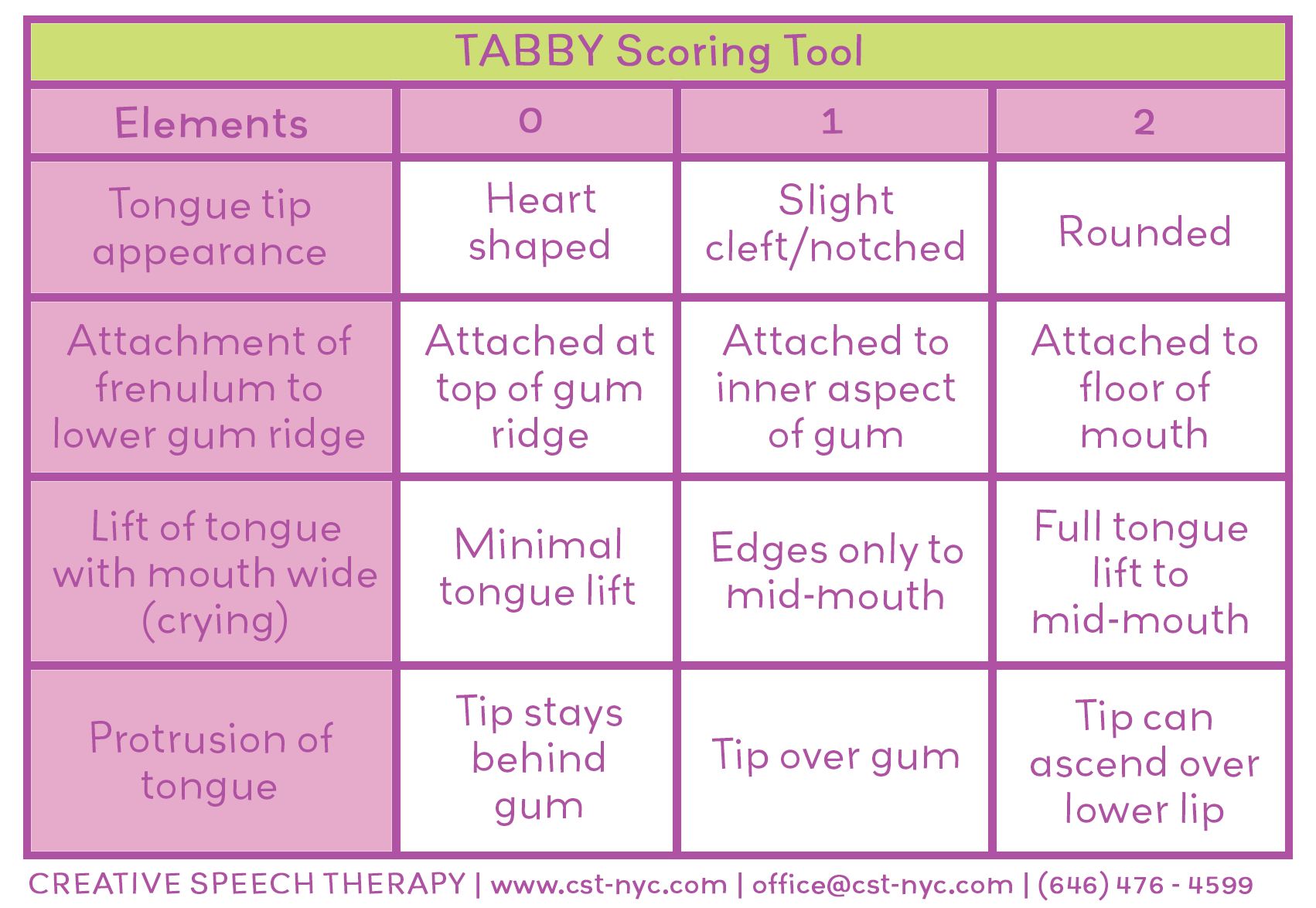
Tabby - screener (include images in the photos file – 2 that start with TABBY)
Hazelbaker Assessment Tool, Kotlow Scale, Martinelli Scale
Torticollis info (Boston Children’s)
Breastfeeding infants with congenital torticollis (NIH, Catherine Watson Genna, IBCLC)
Some articles on the education pediatricians get (or don’t) on breastfeeding/lactation:
Sponsor links:
Free “Pack for Your Best Birth” Packing List (with free mini-course option)
East River Doula Collective (find a doula, attend our free “Meet the Doulas” event)
Birth Matters NYC Childbirth Education Classes (Astoria, Queens and virtual)
*Disclosure: Links on this page to products are affiliate links; I will receive a small commission on any products you purchase at no additional cost to you.
Episode Topics:
Introduction to Rachael Rose, SLP
Rachael’s background as a speech-language pathologist and founder of Creative Speech Therapy in Manhattan
Her passion for infant and toddler feeding, and orofacial myology
What Are Tongue Ties, Lip Ties, and TOTs?
Explanation of tethered oral tissues (TOTs) and their impact on feeding and speech
Anatomy of oral restrictions: tongue tie, lip tie, cheek tie
How fascia and connective tissue play a role
Signs and Symptoms of Oral Restrictions
Common signs in babies: clicking sounds, poor latch, fatigue during feeding, gassiness, reflux, and weight gain issues
Maternal symptoms: nipple pain, need for nipple shields, and feeding challenges
How to distinguish between normal newborn sleepiness and feeding-related fatigue
Functional Assessment vs. Diagnosis
The role of speech therapists in functional feeding assessments
Which professionals can officially diagnose oral restrictions (ENTs, specialized dentists)
Importance of a team approach and collaboration with lactation consultants, doulas, and other specialists
Challenges with the “Wait and See” Approach
Research on delays in intervention and the developmental impact of waiting
The importance of early detection and intervention for optimal outcomes
Impact of Oral Restrictions on Development
How tongue and lip ties affect palate formation, nasal breathing, and jaw development
The ripple effect: from feeding issues to speech, sleep, airway, and even behavioral concerns
Connection between mouth breathing, sleep quality, and misdiagnosis of ADHD
Feeding Therapy and Prevention
Strategies for supporting infants and children with feeding difficulties
The role of exercises, stretches, and myofascial release
Preventing long-term issues like picky eating, need for palate expanders, and orthodontic work
Empowering Parents
Encouraging parents to trust their intuition and advocate for their child
Breaking down overwhelming care plans into manageable steps
The importance of family and community support, even when professional resources are limited
Assessment Tools and Resources
Overview of assessment scales: Hazelbaker, Kotlow, Martinelli, and the Tabby screener
How these tools help guide recommendations and interventions
Case Studies and Real-Life Examples
Stories of families navigating feeding therapy, oral restrictions, and team-based care
The individualized nature of treatment plans
Access and Equity in Care
Addressing financial and logistical barriers to therapy and interventions
Creative ways to build a support network for families
How to Work with Rachael Rose and Creative Speech Therapy
What to expect from an assessment and therapy sessions
Contact information and resources for further support
Final Thoughts
The value of early intervention and prevention
Empowering parents with knowledge and confidence
The importance of a holistic, family-centered approach
Interview Transcript
Lisa (0s): You are listening to the Birth Matters podcast, episode one thirty five.
Rachael (4s): If you look at early intervention articles and studies, the wait and see approach is never the right approach. There's a study that I found recently, the average onset of a child having a feeding issue was three months, but the average age that the doctor actually referred the child for intervention was 19 months. And that's huge in a baby's development. The wait and see approach to me is so detrimental because number one, the baby is learning to use different muscles.
The baby's frustrated, the parents are frustrated and the muscles and the bones are fusing and forming during that time. And if you're feeding however many times a day that you're breastfeeding over six months, that's a lot of time to be using the wrong muscles and overdeveloping some and under developing others.
Lisa (1m 7s): Hey there and welcome to the Birth Matters Show. I'm your host Lisa Graves Taylor, founder of Birth Matters NYC, and director of East River Doula Collective. I'm a childbirth educator, birth doula and lactation counselor, and I've been passionately supporting growing families since 2009. This show is here to lessen your overwhelm on the journey into parenthood by equipping and encouraging you with current best evidence, info, and soulful interviews with parents and birth pros.
Please keep in mind the information on this show is not intended as medical advice or to diagnose or treat any medical conditions. If you enjoy this show, we'd be incredibly grateful if you'd share it with a friend. You can follow and share our posts on social media at Birth Matters NYC, or simply tell them to search for birth matters wherever they listen to podcasts. Since the topic of tongue ties and other oral restrictions has come up in several past episodes and also comes up quite a bit with families I work with, I thought it would be helpful to have an expert in the field on the show to share further educational content on this topic.
So our guest today is Rachael Rose, owner of Creative Speech Therapy in Manhattan. We discuss the identification and treatment of tethered oral tissues or tots in infants, more commonly known as tongue ties or lip ties and their impact on feeding speech and overall development. Rachael explains the importance of early detection and intervention to prevent long-term issues, the importance of trusting parental intuition, the need for a supportive team approach and the challenges parents face in getting proper diagnosis and treatment.
Before we hear from Rachael, I just wanted to offer you a free educational resource. Do you have your free pack for your best birth list yet? This is a great way to start some practical preparation for the big day and really start envisioning your ideal birth. All you have to do is go to birth matters online.com/pack to grab it. You'll also have the opportunity to take a free online mini course that will help you more thoroughly prep for a positively transformative birth. Again, that's birth matters online.com/pack.
Okay, now here's my chat with Rachael today. My guest is Rachael Rose. She's a speech language pathologist and owner and founder of Creative Speech Therapy, a practice on the Upper East side of Manhattan. Some respected doula colleagues in my collective had brought Rachael to my attention a while back saying that she's been a really fantastic resource for the families that they work with. And as soon as I met with Rachael, I immediately knew she'd be a great fit to share about the hot topic of what's commonly known as tongue ties and lip ties or the broader and lesser known term of tots, which she'll explain more about in just a few minutes.
But first, welcome Rachael. Good to have you.
Rachael (4m 6s): Thank you so much. I'm very excited to talk to you today and talk about this topic.
Lisa (4m 10s): Me too. Would you please give a little bit more of a detailed introduction of yourself for listeners?
Rachael (4m 16s): Yes. I've been a speech therapist for about 20 years. I opened Creative Speech Therapy about 10 years ago and it's a private practice, as you said on the Upper East Side. And we're a group of specialists, so I specialize in infant and toddler feeding. And I also am an orofacial mycologist, which will come into play later when we talk about tongue tie. And I have a passion for working with babies and children who are having difficulty eating. It feels like a superpower to be able to teach parents how to get over those really stressful moments, especially like young babies.
And if it's just not coming naturally, the mom feels very guilty. And so I like to alleviate a lot of that. And then we also love working with kids. We're transitioning to solids around six months, 18 months is another time where we get a lot of kids and then we also have specialists here who work also on feeding and then also with kids on the autism spectrum. But this is my passion. My area is feeding and anytime a child has difficulty with feeding, we also look at speech because at the end of the day they're muscle based movements and so you're using the same muscles.
So both typically can be impacted. But yeah, I love what I do. I love talking about it and I wanna shout from the rooftops to parents about these things that you can do to help your child and then also prevent, that's a big tenet for me is about prevention. So that's why I'm so happy to be here. Yeah,
Lisa (5m 45s): Happy to have you. And I just sent your information to a client who had her baby recently sec. They had their second baby and they were having, they had identified an oral restriction and they weren't having any issues with breastfeeding thankfully, but they still knew that, they needed to address it. And so they asked specifically for a speech language pathologist and I was like, I have somebody for you. Let me send you this wonderful resource. So hopefully they're getting in touch.
Rachael (6m 17s): No, that's amazing. 'cause I think a lot of people don't know that speech therapists do this type of work. Not all of us do, but I think sometimes parents don't even know that this is a resource that's available. So I love that you're, you know, you're knowledgeable too and sending them our way. Yeah,
Lisa (6m 30s): And I knew, I love that they knew to ask for that. Alright, let's just jump right into it 'cause there's so much that we have to talk about that we, I want to talk about. So first, let's start with the basics. Can you tell me what is TOTS?
Rachael (6m 44s): Sure, yeah. So we use the word TOTS because there's actually more than one place for restriction. Essentially we have a connective tissue around all of our muscles that's called fascia. And you think of it like the fabric of your body. So it's connected to everything. So if there's a restriction in one area of that fabric, like if you were to pull fabric, you can see that the wrinkle kind of occurs and somewhere else in the fabric it's gonna be pulled to. So what TOTS are is they're fascia that connective tissue and in the mouth there's seven points of connection.
There's a connection between the upper lip to the upper gum, the bottom lip to the bottom gum, the tongue to the floor of the mouth. And then you have four cheek ties or four points of connection, two top points and two bottom points. And in utero these you, your babies are typically more tight and then at a certain point they release. And when the baby is born, they have maximum function. However, sometimes it doesn't happen.
And that's essentially what tots is. It's a restriction that is gonna prevent a child from being able to move that part of their mouth the way that it needs to move. So if you have a tongue tie, it means that the tongue can be tethered to the floor of the mouth. So if you're nursing, you can't get that bottom seal where the tongue has to move over across the bottom blip to create that nice seal around the bottom of the nipple. So if the tongue can't do that, then the baby's gonna compensate. And that's where the problem lies because then they're using different muscles.
They might be chomping, we can get into signs and symptoms, but the baby's gonna try to compensate for that restriction and use other muscles or just struggle. Similarly, if the upper lip is tethered to gum or the teeth, then the upper lip can't flange around the nipple on the top to create a nice seal there. As the way the babies form when they're born is their tongue should be resting on their palate on the roof of their mouth. And that's actually how the roof of your mouth is shaped is how you as a baby rested your tongue.
So while you're listening to this podcast and you're listening to me talk, most likely your lips are closed and your tongue is resting on the top of your mouth. That's a nice healthy way to be listening for a baby. If the tongue is tied to the bottom of the mouth, it can't actually rest on the palate. And those bones haven't fused yet. Just like you have the, the spot on the top of your head, your palate, your palatal bones haven't fused. And so what happens is the palate tends to grow up and into the nose and the nasal cavity and then that's gonna cause breathing problems that we can definitely talk about later.
So depending on what is tied, it's going to impact feeding in a different way. And then also depending on how it's tied. So we look at two factors. The first is where is that piece of frenulum, that connective tissue, where is it connected to? If it's connected to the wrong place, then you might need to release that. If it's thick and fibrous, then you're not gonna have as much movement. So then you might wanna look at a release too. What I always recommend is going with a functional assessment so that you can look at, it's one thing to know that there's a tie, but there's another thing to look at like what is functionally happening with the baby and feeding and how is it impacting because it doesn't always have to impact feeding necessarily.
Lisa (10m 25s): And between a tongue tie, lingual, upper lip tie labial or a buccal tie, an inside cheek tie, what do you see as the most common? I know my perception, but I'm curious in your field.
Rachael (10m 39s): Yeah, no, that's a great question. I would say I see a good amount of tongue tie and because I think that's more obvious to parents, I think you can, sometimes you can it. That's what I was thinking. And oftentimes, yeah, and I think oftentimes it, it impacts greatly in a way that feels like, oh, that's pretty obvious. I can see it. I'm feeling that I'm not getting a good latch. Like that kind of thing. But I also frequently see upper lip tie and that to me is missed more often than tongue tie because babies can compensate for that better just because there's surrounding muscles that they can use as opposed to the tongue as a free floating muscle.
So if that's tied then there's not a lot of other muscles you can use. But if it's an upper lip tie, then I think it's easier to miss if you're just like a parent. But I think the impacts are not as widely known. It's pretty rare that I see a cheek tie, but I have seen them and they do impact, I would say tongue, then lip, then cheek would be my grouping there.
Lisa (11m 40s): That was my impression. Thank you. Yeah. So what about science? How do we know both in babies as well as parents, the mom, what is right, how are, how do we know?
Rachael (11m 53s): Yes. Again, you can look at the structure, the average person, it took me a long time to really learn how to diagnose and we don't diagnose, but how to measure and all of that. But I would say looking at functional impact. So some of the hallmark signs of a tongue tie for example, are for the baby's side. You might hear clicking noises. That's a pretty hallmark sign. Essentially what that means is they're trying to use their tongue and other muscles to get the milk in. And so that makes like clicking sound, often those babies are gonna get really tired after they have nursed for a little bit.
So they might fall asleep or just fatigue and fall off the breast. And that's again, because they're using muscles, they're not supposed to use these, the muscles were not meant for that. So those muscles get tired and the baby's working so hard to drink the milk that they actually get tired. Another sign would be from the mother's. So there's maternal signs too, nipple pain, needing to use like a nipple guard. If you feel like they're biting on the nipple, that's really painful. And that's a pretty good sign that they're not able to get a nice suck, swallow, breathe synchrony.
And so they're moving up and their jaw up and down to try to get some of the milk out. And then medically, those can be kids who are not gaining enough weight and not reaching their height and weight curve milestones. And again,
Lisa (13m 15s): 'cause they're not getting enough milk, they're not able to correct.
Rachael (13m 18s): So when we eat, we like to expel more calories than we take in. We say that's fitness, but when babies eat, they need to get more calories in than they are using. And so they need those extra calories to grow. And so they need to get as much nutrients and in them in a short amount of time in order to be able to grow and thrive and all of that. So babies have an opposite problem than we adults do.
Lisa (13m 45s): I never thought about it that way, but that's a great way to frame it. Yeah, I feel like some of the signs are ones like, I feel like it's more known by a lot of new parents of the clicking sounds poor latch. But things like falling asleep at the breast, like that's a sign that they're exhausted 'cause they're having to work too hard to get the milk. Although that's tricky though in the first two weeks because in those first two weeks they're so sleepy and chill that that's, I feel like, would you say that's more a sign?
I don't know what any comment on that specific point.
Rachael (14m 23s): Literally as I was saying it to you, I was thinking about that point too. I would say, yeah, the first couple weeks babies are so sleepy, they're sleepy and you're seeing some other signs. That's when you know that it's not just a sleepy newborn. If they are having gastro problems, that's another sign. So very gassy. So think about if you have a weak latch, you're getting a lot of air in and then the tummy is filling with air instead of milk. And so they're gonna feel full faster. But
Lisa (14m 51s): Also those are ones that are lesser known too. I feel like the gassiness, the colic, the reflux symptoms kind of stuff. Yeah,
Rachael (14m 57s): Yeah. Oh, to know.
Lisa (14m 58s): Yeah, absolutely. Because it's so common. So common.
Rachael (15m 1s): So common. Meet
Lisa (15m 1s): Any new parent and they're like, my baby's gassy.
Rachael (15m 5s): And what's, there's so many reasons why, you know, like this could be, so it's essentially, it's a combination of symptoms. So there's some hallmark ones like for example, if your baby has acid reflux, the hallmark sign is a really wide arch of the back. Not just pulling off but really arching your back off of the nipple. And so if I hear that's a red flag to me, I want you to go see the doctor, we need to make sure that there's not contents coming back up. 'cause that's painful. So it's like that, like anything in the world, right? Like you wanna look at the combination of symptoms, look at the whole baby, look at how they're doing in general and then whittling it down to the top things that are impacting their feeding.
So like I said, not tongue tied lip tie. That doesn't always have to impact. They have to work a little harder. But a lot of babies can do better, even with just the stretches and exercises that we as speech therapists can teach without having to go the route of surgery first.
Lisa (16m 1s): And can you just clarify for listeners, when you said you don't diagnose, and I know like lactation consultants also don't diagnose, they can identify and suspect and recommend to get it assessed. Can you clarify what are the different professionals who do diagnose officially?
Rachael (16m 18s): Yeah, absolutely. So we refer either to an ENT or to a dentist who specializes in this. And something that I would say to all parents is find somebody who does this exact thing, right? Like in anything in life, like you wanna find that doctor who does tongue tie all the time, or a speech therapist who's doing infant feeding and sees these babies all the time because they just, they've seen it. They know the resources, they know what to do. So what we do is we do a functional assessment, which what speech therapists do is we do a functional assessment of the infant reflexes.
'cause eating the first six months of life, it's just babies using their reflexes. They're not really choosing to eat or not, they're using a lot of those reflexes. So we're looking to see is there a reflex that's maybe not developed enough? If so, we'll teach the parents how to improve that reflex. And then we do a functional feeding assessment. So I'm looking at the tongue, the lips, the jaw, how they're all working together. I'm seeing how the baby's feeding and then I'm talking the parent through what is going on and then how we can fix it.
And then the third part is I look at the baby. So there's a lot of interventions that we can do to look at how pliable their cheeks are, if their lip is tight, if their tongue is tethered. So we look at the structure, but I also look at the function. So I'm stimulating some things and doing some stretches and exercises so I can get those muscles to work the best they can. Then we teach those parents those exercises and then we follow up. And if after that they're still not seeing really great results, then we would refer to an ENT or a dentist.
And I'd like to send a letter to that professional so that they know what the functional impact in that child's life is. Because I think that's really important. Again, structure almost doesn't matter to me. It's about the day-to-day life of the parent and the baby and getting that connection as early as possible between the family and the baby. I can measure it. And we have scales that we use. There's a scale that we use for measuring the amount of tongue tie, the amount of lip tie. And so we use assessments like that here.
But I'm not the professional to diagnose. I can provide a really detailed plan and recommendation for the doctor.
Lisa (18m 43s): And do you ever come up against the challenge? I have heard about a lot from lactation consultants about pediatricians and their, it is, my impression is that pediatricians and my experience has been that pediatricians have been pretty reluctant on average to say, to say, yeah, this matters at all. Maybe they have, maybe they say yes, this, they do have a restriction, they do have a tie, but it doesn't actually impact breastfeeding. I just wanna take this moment to do a PSA to say that I have had pediatricians in class who have told me they get zero and maybe up to three hours of education on breastfeeding in medical school.
And so unless they have gone the extra mile to do continuing ed, to really educate themselves on breastfeeding, they really don't know. And I've had so many tell me, yeah, we, we really don't. My pediatrician, our family pediatrician office, I was so excited, just hired two pediatricians that HA have their I-B-C-L-C. So I was like, oh yay. I can be more confident that they're gonna get good breastfeeding advice. But do you see that clash at all in the work that you do?
Rachael (19m 54s): First of all, that's fascinating. I did not know that's how little pediatricians got in this area. Yeah, and I absolutely, I get so much pushback, a wait and see approach, which if you look at early intervention articles and studies, the wait and see approach is really, it's never the right approach. There's a study that I found recently that was conducted in Canada and they found that the average onset of a child having a feeding issue was three months.
But the average age that the doctor actually took it seriously and referred the child for intervention was 19 months. So there's a 16 month gap. And that's huge in a baby's development where they have any kind of feeding issue. It doesn't have to be related to tongue or lip tie. Hmm. But there's yeah, that wait and see approach to me is, it's so detrimental because number one, the baby is learning to use different muscles. The baby's frustrated, the parents are frustrated, they're not forming that amazing bond that you get from feeding your baby.
And that's how babies regulate their sensory systems. And so you're, you have all that time and to not intervene and the muscles and the bones are fusing and forming during that time. And if you're feeding however many times a day that you're breastfeeding over six months, that's a lot of time to be using the wrong muscles and overdeveloping some and under developing others. And so it's frustrating to me what I, one of the reasons I love coming on your podcast today is to just even empower parents to say, this doesn't feel right in my gut.
Lisa (21m 37s): Trust your intuition. Yeah.
Rachael (21m 38s): Trust your intuition. Yeah. And find, dig deep like you just said, maybe they don't know as much as we think we trust doctors, they're wonderful. But if they're not specialized in what you're talking about, they may not have that knowledge but they might feel pressure to give you an answer. Yeah. Which is usually wait and see.
Lisa (21m 56s): Yeah. Yeah. And I absolutely hear it in a minute. Wanna take a deeper dive into why early detection matters so much, which you're already starting to talk about a little bit before we do. The other thing that came to mind when I brought up the pediatrician dissonance was this New York Times article that was, that came out in the last year or so that you and I discussed a little bit before we hit record. And we both were really frustrated with what a bad wrap, getting tethered, oral tissues, tongue ties, lip ties, so forth, getting those assessed and corrected.
It just got us such a bad wrap and it was really frustrating because this is such an important thing to address when necessary. When I do know at least one, I know one client, most of my clients who've gotten an ectomy and body work and, and all of this one or more of those things have been like that was a game changer. I'm so thankful I did that. I did that. I did have one client couple who were very unhappy with, they were like, they felt like it was trauma that it caused their whole family and, and they, so they were glad when that article came out.
But I know we'll talk about how individualized this should be and how we need to empower parents to make the choices that intuitively feel right for them. And there's a number of paths that can look like. So we'll get to that maybe in a little bit. Anyway, anything you wanna comment on all the, all everything I just said? Yes,
Rachael (23m 25s): Absolutely. Yeah. I was disappointed at the time because I think that it takes from people like myself and other professionals who are really here to help families and really learning about this and have taken the time to really get to know this issue. And I think it takes away from that a little bit because in any business, not everybody is as studied up on certain things. I also think that kind of sweeping generalizations about a medical intervention in general are dangerous. I think that you have to look at the child and the family unit and really make a choice that's appropriate for that family.
Yep. In my profession, like with my families, I don't always recommend a tongue tie revision at all. I talk to the family, I look at what their values are, what their expectations are, how difficult it is day to day. And like I said, I can be that middleman to say, okay, I hear that you don't wanna medically intervene with your baby. It feels like it's optional, but here let's try to get maximum function and then take it from there. So I guide our families through that.
I think in the article it really was just looking at people who were just like snipping and not following up, right? Yeah. And that to me is irresponsible. Like you need to, so in our practice, if we're recommending a child to go get an ectomy or any kind of restriction released, we always teach them the exercises and stretches that they're gonna have to do after we teach them before. Because to me, I need you as the parent to be comfortable with this when it's go time when the baby has a wound and feel comfortable 'cause we gotta really get in there and move some stuff.
Yep. 'cause the truth is if you don't do that, it can grow back and it can grow back thicker. So I always tell parents, if you're not ready, let's wait. Like it's better to wait and have you be ready to do all the after work that is needed for, 'cause what we're trying to do is get that lip to move more, to get that tongue to move more, to be able to eat, to be able to speak. And if you don't do the follow up, it's not worth it. So I think in that article what they lacked to talk about was what a good team of a child who has a tongue tie would look like and how that team supports the child as a whole and is not just a factory.
And I do feel like that is irresponsible. Absolutely. But I also don't see that a lot. At least I'm not referring and getting referrals from providers like that. We're a very holistic team here. And so I'm getting from the doula and then I follow up from the doula or the midwife or whoever and then we're all saying, oh this is great or this is not working. How can we work as a team? And I think that to me is the critical piece. I'm not gonna go if I break my elbow, go to have surgery and then not do PT afterward. Totally.
Lisa (26m 19s): Yeah. Same with,
Rachael (26m 20s): Same with the ectomy. You're not, you shouldn't do it and then not follow up. Yeah.
Lisa (26m 24s): Yeah. Absolutely. Yeah, definitely. I do feel, I'm always concerned that this idea that is so important of a team approach tends to maybe overwhelm parents. But like I love that you said you're listening to them, you're getting a sense of their values, where they're at, what's going on with their nervous systems right now. Are they ready to do this extra little bit of work that it requires for it to be effective or not? And also like I of course don't get me started on making things accessible too because this could also be financially overwhelming to people to think about going to get to body work, to craniosacral therapy and after post ectomy and working, doing ot, pt, SLP, all these and any of these myofascial work, there's so many different, several different options for people that could really help their baby to thrive.
Which is all that everybody wants. But I'm just, I always am sitting with that. How do we not overwhelm the families how to, how can we hold space for where they're at and guide them knowing that we know what we know And we were like, it's important but also it's their baby and it's their family and it's their choice. So that's that. I just find that tricky.
Rachael (27m 41s): Absolutely. It makes me think of a family that I'm working with right now and they're stretching their budget to come and see me. Their baby is tube fed and we're trying to get her off of the tube and become an oral feeder. And every week I check in first I just check in how was the week, gimme the overall. And then we come up with two things that I want them to implement that week. And that's it. So whether it's because it's a two from this case, it's a two fed baby, whether it's can you sit and have one meal while you're, while she's being fed so she gets the family meal experience or if it's can you let her be messy?
Let her be messy three. 'cause this mom is one of those cleaning the face and I'm like, there's a really strong hand to mouth connection with feeding. Let her be messy. So we'll come up together with two things that they can reasonably implement that week and then we can either add on or we can shift. But yeah, and for in, in that case too, the mother was not confident in doing any of the stretches. This baby did have a tongue tie but the dad said, oh I got this, I'll do it. And so I taught him all the exercises and we sent videos and he sent videos back and forth and it was a success.
But yeah, to me it's not a cookbook. You have to look at each family and figure out what's right for them. Some parents want a big team, some parents don't. We can give them resources instead of referring to another therapist or something. But yeah, it's just, you gotta look at the family I think honor that.
Lisa (29m 13s): Absolutely. I love that Rachael, that is brilliant to just break it down, keep it simple. Two things that is so smart.
Rachael (29m 22s): Thank you.
Lisa (29m 22s): Because new parents can get, all of us can get easily overwhelmed but especially new parents who are doing a lot for their babies already. It just feels like so much more now that oh my gosh, this opens up this whole can of worms. It feels like up to a lot of people. Oh no, where do we even start? Somebody just give me a roadmap.
Rachael (29m 41s): Yeah, that's exactly And that's what we do. Like when we have the infants come in, I will give, I will teach them the exercises in the office, then we send 'em home with a treatment plan. Again, it's three or four things that you can do now to help your baby. And then we follow up with them and there's, yeah, because I think if you give them everything that they could be doing that is so intense, like it's crazy. And then there's that snowball of, now I need a craniosacral therapist, now I need to know. But if you can also just pare it down, this is one part of your parent experience and here's two things you can do, three things you can do today and have them walk out of my clinic with that knowledge.
It's empowering. And then they feel like I got this as opposed to feeling so sad and what you, instead of feeling the opposite of that.
Lisa (30m 31s): Yeah. Yeah. I love that you're there to help guide them on that and reframe it as there's good news. This is good news that we're identifying it now because the sooner the better. Yeah. Which leads me to, let's talk about early detection. You touched on it a little bit, but I'd love to take a deeper dive into all the reasons why the sooner the better that we can identify if a baby has an oral restriction.
Rachael (30m 59s): Absolutely. So this is where I really geek out. I love talking about
Lisa (31m 1s): It. I love geeking out. Let's do it. Okay.
Rachael (31m 5s): So yeah, so just even going back to the palate and the formation of the palate, for example, when any parent comes to me with their infant, I teach them a massage that you can do to help form the palate. What you want your baby to have and your child to have is a nice broad upper mouth. That palate should be nice and broad because then the teeth fit together and we need to grind our teeth together to chew. And also because that means that they have free space in their nose. There's something called the open mouth ripple effect.
And it's actually now a hot topic breathing through your nose versus breathing through your mouth. And so essentially if you have a tongue tie and your tongue is resting on the bottom of your mouth, you can't form the palate like I mentioned before. The palate grows high and has like a groove and it grows into the nose. It's really important to breathe through your nose because there's little hairs in there that clean all the bacteria and the germs and it filters clean air into the back of your throat. You're doing great. If there's obstruction in the nose, then the body always prioritizes breathing over anything else.
Breathing, overeating, breathing over anything. That's why when you are sick and you have a stuffy nose, you want to eat like soup and not a steak 'cause you can't breathe to eat the steak. Same with kids by the way. If kids are constantly stuffy, they're gonna become what we call picky eaters. And I'm using air quotes, but they're limiting their diet because they truly are having trouble breathing through eating.
Lisa (32m 42s): Wow. I never made that connection before. That's fascinating. And the reason why you were seeing me get all excited visually geeked out was because I just finished this book called Breath. Are you familiar with it?
Rachael (32m 57s): It's on my actual bookshelf back here. Oh, I
Lisa (33m 1s): See a yellow book.
Rachael (33m 2s): Yes. That's it. And yeah, and I'm, we can talk about this for hours but
Lisa (33m 6s): Yeah, I'm about to read it a second time. I bought it now like I loved it so much that I like, oh now I bought the audiobook and the Kindle and I might get a hard copy 'cause I wanna highlight things in it. Talking about yeah, so much of this. And so I have been focusing on the nasal breathing ever since it is so compelling and talks about some of the stuff that you were just elaborating on. And so I'm trying to assimilate what I read in that book with what you're talking about. Yeah. Yeah. Thanks. And
Rachael (33m 34s): That's just the tip of the iceberg too, because the more that you breathe unfiltered air, the more that's going to annoy your tonsils and your adenoids. So now we're getting kids in there at seven or eight and they have enlarged tonsils, they have swollen adenoids, then they can't swallow as well because there's not a lot of swallowing space. And also when we breathe through our mouth, we're essentially you the next book, maybe it's in breathe too, but the next book you should read is called Jaws. The Hidden Epidemic, I think it's called.
The more that we breathe through our mouth, we're actually over breathing. So our blood oxygen levels are getting weird, but also those kids are not sleeping well. So if you have a restless sleeper, if you have a snore, if you have a kid who's waking up in different positions, that kid is not getting good sleep. And it's probably because of open mouth posture while they're sleeping. And a lot of those kids are being misdiagnosed as having ADHD because when kids are overtired, they're hyperactive. Yeah. And that's a whole nother part of it.
Lisa (34m 36s): I started, I had read a little bit about this before this book, but in just enough to know that I do the mouth taping at night. Mm. And I have the nose flare thing because I have had a history of sinusitis and allergies growing up so badly. And I was like, I know that I breathe through my mouth all night long and I had read just enough to know that's really not good for you. Although this book helped me understand at a gut like deeper level for sure.
Rachael (35m 2s): You're like, you can't unlearn it. Right. Once you know it, you're like, oh my god, this is crazy. Need
Lisa (35m 7s): To tell everybody I know.
Rachael (35m 8s): Yeah. And what's amazing is there's no medicine needed, right? Like your kid doesn't have to take a pill, allergies, all that stuff. Like you can, if you're breathing nasally, you're not gonna get as many colds. You're not gonna have to be on antibiotics as much. You're not gonna, there's just so many benefits of breathing through your nose. And the reason it's so important that I see, we see infants and babies is because that can all be prevented. It's just a ripple effect. It's like a snowball. If they have a tongue tie and it's not addressed, then eventually their chin can become recessed and their lips, their teeth misaligned.
I see kids at 10-12 who are getting palatal expanders who are needing a lot of braces and it's all because of the open mouth breathing. And a lot of that, one of the main reasons is related to if your tongue is not forming the palate. And also if your lip is tied up here and it can't close, then your mouth is gonna be open at rest too. So getting a lip released too can help with closed mouth posture. Can I geek out a little more for a sec please? Always please. Yes. Okay. The, it's a new epidemic essentially in our society that started when we industrialized.
So our ancestors had perfectly aligned teeth and they had no cavities. And that is because they were eating meat, fruit, vegetables, grinding foods. And when we industrialized, number one, we moved indoors and so our air is less clean. And two, we started eating a soft diet. Think about especially like kids' foods, like they're all pouches and cookies, soft cookies and chicken nuggets and hot dogs. We call those like pre-processed meats.
So this is a result of our diet. And so I think that's really important for parents to know too. Like getting your kids eating good foods early is really gonna support their jaw development, their airway, all of that. So then the other thing is it impacts speech because speech is also muscle based. So if you have a lip restriction, it's gonna be a lot harder for you to make a P or a B or an M.
'cause you have to close your lips. A lot of times kids will compensate for that by moving their chin up to meet the upper lip. And that causes overgrowth in the front of the chin. There's a muscle in there called the masseter muscle. And that you can overgrow that if there's a cheek restriction, a lot of kids will try to compensate by suckling food instead of chewing food. So I see that a lot important to know, not for the infants, but when you're six months in transitioning to solids, when we're eating, we hold the food on our teeth on one side with our cheek and on the other side with our tongue.
So you have to have motion in those two muscles. There's many muscles, but in those two areas in order to safely chew food, otherwise the food's gonna fall onto your tongue or it's gonna fall into your cheek cavity. And then you have to suckle it down to chew. So I get a lot of, also like six months, seven month olds who do it, like the parents are like, they're real picky and like they're just wanna drink the milk and they don't wanna transition. It's often not that the kids don't want to, it's that they can't.
And that is telling me, the therapist and you the parent, that there's an issue, an underlying issue. Only 1% of picky eating is true behavioral picky eating. The rest of it is typically there's an underlying reason why and it's usually structural or functional.
Lisa (38m 50s): Wow.
Rachael (38m 51s): Yeah.
Lisa (38m 52s): So if a parent just notices that that's the only thing they're really noticing in their child or baby that they seem to be they yeah, they're picky eater so to speak. Would they, should they come to you to be assessed or what? That would be the first best first step.
Rachael (39m 10s): Yep. Because again, there's a snowball effect there too. They perceive that the child is perceived as picky. Mealtime has become stressful, it becomes a battle. And then meaning becomes a trigger for the child to say, uhoh, it's mealtime. Now I'm gonna go into fight or flight. Now my brain's gonna tell my stomach to turn off. And I'm gonna say to my parents, I'm not hungry. When I had just told 'em I was. And then they're gonna think it's behavioral. So the earlier that you can intervene, the better because you can prevent that.
And yeah, a feeding assessment is definitely what you'd wanna do. I would say, and this is just anecdotal and 80%, 90% of the clients that come to me with children who are quote unquote picky, we find there's an underlying issue of why if, and most kids don't want to eat meat and vegetables. And so often parents will think it's 'cause of the vegetables. But often we find that it's because those are the foods that you truly have to grind down with your teeth as opposed to an applesauce pouch or a cracker that's easy to break down.
So these kids are picking diets, a waffle, a scrambled egg, they're picking diets that they can easily chew and it has a ripple effect. Number one, the parents think they're picky, but two, now they're not chewing and developing their jaw and now they're getting into the airway issues. But for infants, it's great to see them at that level, at that age because then I don't have to see them at six months or at 12 months or 18 months 'cause we've prevented all of that from happening. And then the parent child relationship again is solid.
And so my goal in life is to prevent this ripple effect for as many babies as we can. Because it's just, it's eating together and having it be pleasurable is such a wonderful experience for families. And if it's stressful then it's something that you dread at least three times a day and that's bad.
Lisa (41m 5s): Yeah, absolutely. Goodness. And so with a feeding assessment, I'm assuming you're witnessing, is that what that,
Rachael (41m 16s): So in babies it's an assessment of their reflexes and then we look at the structure and then I'll say to the parents, see that this is inserting in between the teeth. That's considered an upper lip tie. Here's what we're gonna, some stretches we're gonna do. Then we do a feeding assessment and I say, okay, here's these signs and symptoms. Here's the plan for an older kid, depending on their age, we have the parents bring in foods of different textures. This is, I guess off of the birth topic, but picky eating is almost always about texture.
There's a very finite amount of smells and a finite amount of taste, but texture is what's off-putting for most picky eaters. Or it's a texture they can't eat. So we have parents bring in a puree like an applesauce, a crunchy dissolvable like a cracker, something chewy like meat or a vegetable or, and then something that's a soft solid like an egg or, and we, within their family diet, so I say bring typical foods that your family eats and then we do an assessment of how that child is chewing and swallowing the food.
So we're looking at a bunch of different areas, but how do they break it down? What muscles are they using? And then how are they swallowing it? Because if they're using the incorrect muscles, then we're back into the cycle. And for those kids, they're still young enough too often that with just some training on how to truly chew food and swallow it properly, then they don't get into this ripple effect. So we can prevent it there too. And we use non-food tools to teach chewing skills so that they don't choke.
So there's lots of tools that we have in the field. So there's a subs field of speech therapy called oral functional. My biology and I, myself and our therapists are trained in that. And that's looking at how the interplay between muscles, it's looking at the interplay between muscles and how they work and function. So if you are suckling a food and your tongue is moving front and back then you're using, you're putting pressure on the front teeth, you are, you're using an incorrect swallow pattern. Food's most likely to go to fall on the back of your tongue and you're gonna swallow it accidentally.
So then you're looking at aspirating. So we teach kids how to move their tongues in different ways and how to swallow correctly as really a preventative measure for what could happen later
Lisa (43m 37s): Is all so fascinating.
Rachael (43m 39s): I'm so glad.
Lisa (43m 41s): I love it. This actually got me thinking, and I might edit this out because this is a me question. Tell me it's not a baby question. Not a parent question. Even though I've had babies and I am a parent, I've always had this, I feel like I've had this propensity to, when I swallow it often goes down the wrong, the in like into the wind pipe, wrong pipe. And I'm choking and coughing and mouth breathing. Could it affect something along those lines? I don't know. I just, I never thought about that. Yeah,
Rachael (44m 12s): Anytime a muscle is laying dormant and you're not using it, it's not gonna work as well. Yes. So what I would recommend for you is, especially like if it's later at night and you're feeling tired or fatigued, drink through a straw instead.
Lisa (44m 26s): Okay.
Rachael (44m 27s): Drinking through a straw, especially like a smaller one, you have to, your muscles have to fire more to get the liquid down. Okay. So your cheek muscles. And so it helps trigger a swallow, huh. So we have, you have a swallow that you initiate and then once you do the re it's like the rest of your body is doing the rest of it. And there's, they're triggering different swallows at different points. Hmm. And so if you triggered a swallow but your esophagus didn't know you did it, that's why you're getting it down the wrong pipe.
So if you slow the, and we do this with babies, we'll say go on a thickened liquid or you drink from a smaller straw, if you slow how fast the liquid's going down, then it'll trigger the automatic non volition swallows that your body has to do. My mother-in-law was having issues with that and I put her on a straw and she's been doing better.
Lisa (45m 20s): Wow. Thank you for the tip. It's great. But yeah, yeah, just thinking, yeah, thinking about all of the interconnectedness on all of this. So that's so interesting about that getting this addressed where present earlier as an infant before they're transitioning to solids can really make a big difference in that whole, their relationship with food maybe and your parents' relationship with their little ones in a really big way. Oh wow.
And then also the, you were talking about the palate and I don't know if you mentioned the braces thing, I know you alluded to it at some point, but do you wanna elaborate any more on that?
Rachael (45m 60s): Sure. So going specifically to tongue tie, if you look at your baby and they have a little band of skin that's going around and behind where the two front teeth would insert would come out, that's a, a upper lip tie. And what would happen is once those teeth come out, there's gonna be a space in between them.
Lisa (46m 18s): My son had that and I, we never had him assessed, but now I'm like, maybe he had a lip tie.
Rachael (46m 25s): Yeah. And listen, I walk around with cheek ties. I personally have 'em and I compensate for them and I'm doing fine. So again, it doesn't have to be, but it depends on how restricted and where I am able to function. But, so it, going back to, wait, your question was, and I've lost train of thought,
Lisa (46m 43s): Just anything you wanted to expand on about eliminating the need for future braces possibly, and you did touch on it some, so it's okay if you don't have anything extra to add to that.
Rachael (46m 54s): I think the only thing to add would be if the pallet is not high and narrow, then you wouldn't need a pallet expander. So we do work with kids of that age. In fact, I have two on my caseload right now who are older, they're 10 and they're having to go through palate expanders and it's painful. And then their speech is compromised while the palate expander is in there because there's more stuff in your mouth. So then we're working on speech through, through while they have that expander and then feeding while you, 'cause you have to move your mouth a little differently. It's just if that palate is formed as a baby, then you don't have to address any of that.
And it just, it's just so preventative. We can address it from different ages, but it's best if we can address it from infancy. And I would say to parents again, like if you feel like someone said, look, let's wait and see, or just give her a week or two and maybe she'll grow out of it, but your gut is telling you that something's not right. There's a reason for that. I think parents know and it's about finding the right people who hear you and who can either refer you to someone who knows more about that or who can treat it themselves.
But I just feel so bad for parents who do, they get a lot of misinformation right at the front. Different professionals are telling them different things. I get a lot of parents who come to me and said in the hospital, they said it looked like there might be something like a tie, but they didn't think it would impact and yet we've never had a successful feed and she's three weeks old. So it's like that, it's like how do parents know? So that's why I love talking to you today to demystify some of that. And really to me the answer is looking at the functional impact and that's what you wanna address.
Lisa (48m 36s): Yeah. That reminds me of pelvic floor therapy and some of how approaches to things like diastasis recti have evolved over time to really focus more on function than form, than the actual physical state of things. Yeah. Yeah. That's kind of, I think that makes sense because what we need in life is to be functional, right?
Rachael (48m 57s): Yeah. It doesn't matter if you have a, you know, like yeah a cheek tie like myself, I can function with it then that's great. It doesn't impact me. But if I was snoring every night and not getting a good night's sleep and that's a big impact and I can't do my job well and I can't be a good student if I'm a child and maybe I'm not even regulated to eat lunch and all the hosts of things. Again, eating is so from a sensory perspective, it's so regulating, it's so orienting, it's so for the baby, it's self-regulation. And so that starts those synaptic connections in the brain start from infancy and if you struggle then the connections in your brain are telling you as you move on with different foods, I don't enjoy eating or eating hurts or eating is hard.
And so we don't wanna further and strengthen that thought and that relationship. We want to prevent it and change it.
Lisa (49m 53s): Thank you. One question I have is there are different degrees of severity, right? So do you find that sometimes parents can just do work with just you and not have to have an oral revision, a surgical revision, ectomy or cranio? Can they have craniosacral therapy? What are your thoughts on that and experience on that?
Rachael (50m 20s): Yeah, great question. Every family is different and unique. So I really get to know the family as much as I can. Rarely do I have a child, I had a child two weeks ago who came in and I said, this is really tied, it's really tight. I'm going to give you these stretches and exercises, but I really think it's gonna come down to getting a release that's rare for me to go first step. So like I said, there's assessments and measurements, so depending on where that piece of frenulum is attached and depending on how restricted that part of the mouth is, I would make recommendations based on that.
But almost always, at the very least, I teach them a few exercises to try to do a myofascial release. For example, some stretches you can't stretch fascia, but you can work with the muscles around it. So we can look at getting more function out of the lip, more movement out of the lip. Often I'll say to parents, do these before the daytime feeds so that the child has most function and movement before eating and at night nobody has time for that
Lisa (51m 29s): Or energy. Yeah.
Rachael (51m 31s): Or yeah, you just gotta get the baby a dream feed is fine, but then, yeah, and then depending on looking at the whole baby, I might refer to, yeah, like a body worker of some kind. I, and then again, like I always follow up with whoever referred to me and make sure, 'cause I might be recommending different holds for feeding the baby based on reflux, based on gravity, based on restrictions and, but I also wanna talk to the I-B-C-L-C and say, listen, this is what I would recommend, but there's other factors too.
What do you recommend? The other thing that's been ingrained in me for years through continuing education about feeding is whatever's happening in the body is happening in the mouth. So if your baby has torticollis, it might be outta whack in the mouth too. Yep. A baby chiropractor, somebody could be working on that. If your baby has low tone, then they're gonna have low tone in the mouth, most likely. Not always, but typically. So I like to look at the baby's body as well and get information from other body workers, other OTs, other professionals.
And they might say to me, this X, Y, Z is going on. And I'll know that gives, informs me to look at those things in the mouth too. And then give some recommendations globally for the family too.
Lisa (52m 47s): That just really drives home, again the team approach and how important it is because we're all getting different pieces of the puzzle, right? So if we can collaborate, boy can we improve the way we're caring for families. Yes.
Rachael (53m 1s): And when you said that, it made me think, one of the things parents use me for a lot is they'll say, my mother or my mother-in-law said you gotta do X, Y, Z. And I'll say, I'll be the middleman. Let me be the, let me tell them what my professional opinion is and then you're out of it. Bring grandma, bring grandpa, let's talk about it together and beautiful buy from everybody. Let's talk about how we can make this the family, the beans that grandma makes, let's make 'em a texture that's appropriate for the baby or for your child.
I get everybody involved. Yeah.
Lisa (53m 35s): That is beautiful.
Rachael (53m 37s): Yeah.
Lisa (53m 38s): I did also wanna ask about the different skills, the tools, evaluation tools. You had mentioned several, a couple of which I was familiar with, but the other couple I wasn't. Can you just explain a little bit about those tools?
Rachael (53m 49s): Sure. So we have, we have scales that we use to measure and for babies it's more visual. I look at where, so that's not true. I use an upper lip tie scale that that I, that tells me like if it's inserting tear versus here there's four level places of insertion for the upper lip, there's normal, then there's like above the teeth, then there's between the teeth and there's around the back. So that one's the worst or the most restricted. Based on that we, the field has done enough research to know I can make predictions about what's gonna happen with that baby based on that tie.
So if it's a, if the lum is inserting all the way behind the teeth, that upper lip is probably gonna look bowed like a bowed upper lip and pointing out a little bit. And that baby in the future is most likely gonna have a hard time closing their lips at rest and closing their lips to make sounds so I can make some predictions based on research and make some, yeah, some recommendations based on that. For the tongue, I usually use the Hazelbaker assessment.
And again, we're looking at, you know what actually would be a great resource for your listeners is there's something called the Tabby, which is an assessment as a screener that I just put in. I just taught a class to doulas about tongue tie and I put the Tabby in there and it's just parents would, it'd be great for parents actually. So it looks at the tongue along three planes. One is the appearance and you, it gives you a picture. If it looks like this, you give it a one. If it looks like that, you give it a two.
And then it looks at when the baby's crying, I always use when the baby's crying to look at the tongue, how fat, how much can it curl back? And so you give it a score. And then the third is how much can the tongue move out in front of the lip? So those are all things babies need to do to eat. And based on that score, it says to you, okay, you should see a feeding therapist, you're on the border, you know you're fine. So we can put that in the resources.
Lisa (55m 57s): Yeah, thank you. And I am, I'm thinking it'll also be helpful. I'm gonna look through my resources and maybe run some things by you to include other, some other resources. I think it might be helpful for some folks to be, see some visuals, for example. Yeah, thank you. I don't know if I'm familiar with the Tabby screener. I'll have to check that out.
Rachael (56m 14s): Yeah, it's really cool. They have a breastfeeding one as well that I think, yeah, like professionals who are working with infants. It's just a great way, I like numbers around things because it feels just organized. I like
Lisa (56m 26s): That. Yeah.
Rachael (56m 27s): So for babies, I feel like the tabby would be great. And then for older kids, I'm actually measuring how much they can open their jaw, how much they can lift their tongue up. And then I'm writing down those measurements. I'm also looking in the back to see if their tonsils are swollen, if their adenoids are swollen. And then, yeah, making recommendations based on that. The other thing that can happen if you have a tongue tie is because it's in the mouth, it can sometimes pull, we talked about fabric stretching in one area. And then, a lot of kids will report pain in the neck and a lot of them will end up having hunched over kind of head because head hunched over the shoulders because of that push and pull that strain.
Wow. And adults who have had tongue tie releases report that they immediately feel a relaxation in their neck and their headaches go away. Quick aside. Yeah,
Lisa (57m 22s): No, that's powerful. This is so much powerful stuff. Phenomenal. So these scales, I'm not sure if you mentioned all the names. You said Hazelbaker. Kotlow, is that how you say his name? I know that one I've heard 'cause I've followed some of his work. But then Martinelli scale I, that one I also wasn't familiar with. Yeah. Which one is that for?
Rachael (57m 44s): So that is for tongue tie as well. I don't use that one as much. I typically like Hazelbaker, Hazel and Palo. But that said, some kids need different things. So those are like my back burner. I got my front burner and my back burners. Sure,
Lisa (57m 57s): Yeah. Yeah. You don't always need all of the things, right? Yeah. And over time you figure out which ones you like better. Exactly. That work better for you. Nice. Great. So are there any other things, while I'm thinking about if I have any other questions that, anything you didn't share that you wanted to share as we start to wind things down?
Rachael (58m 18s): I, the only thing is I just would like, I guess just about parents, like you were saying before, there's so much to think about when you're a new parent and there's so many people telling you so many things. I just wish there was like a good way to wrap it all into one, one tool. One piece of advice. I think the thing I would say is even if you can't afford a big team of chiropractors and all this stuff, make your family, your team if you can. So rely on, I'm an aunt, I help with the, my nephews rely on the neighbor who's so giving rely on grandparents like that.
Those people can also be really supporting and helping. Sometimes they're giving advice, like I said, that may not be the best, but they always come from a loving place. And so yeah, if you can't, if you can't find the professional team, do your research. We have lots of resources. For example, on our website for parents, there's support, like mommy's support groups on Facebook. Those are great ways to get other ideas. But I would say try to build your internal unit as well.
Lisa (59m 26s): Love that. That's great. And if people are interested in working with you, can you please share here and then I'll also include it in the show notes, how they can get in touch.
Rachael (59m 34s): Sure, yeah, absolutely. We have a website, it's www.cst-nyc.com. You can call us at (646) 476-4599. And you can check out our Instagram. We post a lot of good information about tongue tie there. Yeah. So you can call us, email us, anything like that. And like I said, what we do is we have you complete intake paperwork, we analyze that, we talk to anybody on your team that is useful.
And then our assessments are about an hour. And we're talking you through as a parent the whole time. Yeah. And again, we work with however, whatever's most comfortable for parents. So if sometime we look at parent goals, is your goal to, to try to solidly breastfeed only? Are you looking to maybe go back to work and you wanna add some bottles in and you wanna figure that out? Demystifying a lot of the things that we talked about today is definitely part of our assessment, but we really like to handhold you through it so that you feel really confident and comfortable.
Like I said, I want every family who leaves to feel like they have a tool to empower them to do something about this. Now, not in a week, that's too long. To me you have a two, two week old, three weeks is too long. I need you to be able to do something now and feel inspired and confident and help, like you've really gotten some help. And then, yeah, then we follow up. And usually it's no more than a couple of sessions if at all. Some. That was
Lisa (1h 1m 12s): My next question. Yeah, you
Rachael (1h 1m 14s): Do it. Some parents, we give them the initial exercises. I'll follow up in a week. They'll say, listen, everything's going great. Thank you. And I'll follow up again one more time. And then some families have to come in a couple times to tweak some of the exercises. Or maybe if they're not quite as comfortable doing them, they want a refresher. Or if they've tried our interventions and it hasn't worked the way that we needed it to, then we'll say we have to do a further intervention, which is a release, and then we'll teach them the post-release exercises there.
So it's not a long process coming here.
Lisa (1h 1m 50s): That's really good to know. Yeah, I, because I haven't really had in my resources, surprisingly, speech language pathologists, I didn't, I wasn't so familiar with how many appointments it would be though. I'm guessing as kids get a little bit older, they're no longer infants and they're starting to develop their speech patterns and everything. Is that sometimes longer term work?
Rachael (1h 2m 20s): So yes, I was telling with an
Lisa (1h 2m 22s): Infant, you were talking about infants. Yeah, infant. That's where my brain was then because I sometimes we have people listening who are having their second and they already have a five-year-old, for example. Yeah. So
Rachael (1h 2m 31s): Yes, it really depends on how early I get the child. So for an infant, it's like a couple sessions. Oftentimes we'll get six month olds transitioning to solids. And that can be, that'll probably more like 10 sessions. As the children get older, they need more intervention because feeding is impacted, speech is impacted, airway is impacted. And so there's habits.
Lisa (1h 2m 55s): Now
Rachael (1h 2m 55s): There's habits, there's solidly formed. So those kids are gonna be here for quite a bit longer. Another
Lisa (1h 3m 2s): Great selling point for early detection. And it's in treatment,
Rachael (1h 3m 5s): It saves you money in the long run, right? Yeah.
Lisa (1h 3m 8s): Money in time
Rachael (1h 3m 8s): If you don't have, yeah.
Lisa (1h 3m 10s): And like conflicting school schedules later on where it's so hard to schedule.
Rachael (1h 3m 16s): Yes. Yeah. Yes. Like we're, our schedule is typically very full in the afterschool time slot because that's when we're getting all these picky eaters and teaching kids then. So yeah, in the morning we love to see the infants and yes, I think maybe in the end you probably do save and you certainly save on your child's health and wellbeing, feeding and colds and doctor visits and all of that. Yeah.
Lisa (1h 3m 39s): Really compelling. Thank you, Rachael. What a pleasure. It has been. I cannot wait to share this with everyone 'cause I just know it's gonna be so instructive, so helpful. Yeah. And I hope people, if they're having any concerns at all about their little ones, whatever their age, that they will come to you with those who can, those who are local.
Rachael (1h 3m 60s): Yeah. Oh my gosh, thank you. It was so fun to chat with you and just geek out over all this stuff that I love to talk about. And thanks for giving me a place to do it, to try to reach more parents. 'cause that is, like I said, if I could shout it from the rooftops, I absolutely would.
Lisa (1h 4m 16s): This is the way of doing it. So this be like
Rachael (1h 4m 17s): We're shouting from the rooftops. Yeah. Yeah.
Lisa (1h 4m 20s): All right. Thank you so much again, and have a great day, Rachael.
Rachael (1h 4m 24s): Thank you. You too.
Lisa (1h 4m 26s): All right, so that was Rachael Rose. Thanks again, Rachael. It wasn't that fascinating. I just really, really, really enjoyed our chat. In case you're not familiar with the term torticollis that Rachael used, it's a common condition that can be positional or congenital. When I say positional, here's an example. Sometimes in the birthing process, a baby can get crimped a bit in the position, plus the pressure of contractions and of descending can cause some neck tension and misalignment.
When this happens, the baby has not only tension, but discomfort or pain due to the misalignment and will hold their head a bit crooked instead of centered due to the tension. One thing it can interfere with is breastfeeding, for example, in breastfeeding or body feeding. If a baby favors one side and seems to reject or gets fussy on the other, that's one possible sign the baby has torticollis and could benefit from some body work with someone like Rachael or another body worker, such as a physical therapist or occupational therapist, a craniosacral therapist or a Webster certified chiropractor.
A link to some information on torticollis in this episode's show notes. And I'll also link to some information in the show notes about the modality that Rachael mentioned. Orofacial my, okay, here's a sneak peek of what's up next time. And we,
Kristofer (1h 5m 50s): We had already been thinking about working with doulas, but when this was happening and they were just so dismissive of her pain, I got pretty frustrated and I was like, I, I think we had already engaged our doulas.
Karen (1h 6m 1s): Yeah, we knew pretty early on we wanted to hire a doula. And honestly, hiring a doula was the absolute best decision we made for my pregnancy because that opened up so many doors. It opened up the door to meet you, Lisa, and take your class and just so many resources. And so yeah, it took them almost nine months to say, oh, you have fibroids. Like I was bleeding so much for my periods, I was anemic going up a flight of stairs. Took the wind out of me. That's how Ill I was until my doctor was like, oh, maybe we should do an ultrasound. Oh, you do have fibroids.
Lisa (1h 6m 31s): Thank you so much for listening to the Birth Matters podcast. Dear listener, you are why we are here. So we just want to, on behalf of East River doulas and Birth Matters, we want to wish you a very merry Christmas. Happy Hanukkah, happy Kwanza, happy holidays to you and yours, and we look forward to seeing you in the new year.